Frequently Asked Questions
Obtain scientific expert advice on your COVID-19 questions to help dispel misinformation and myths about the disease.
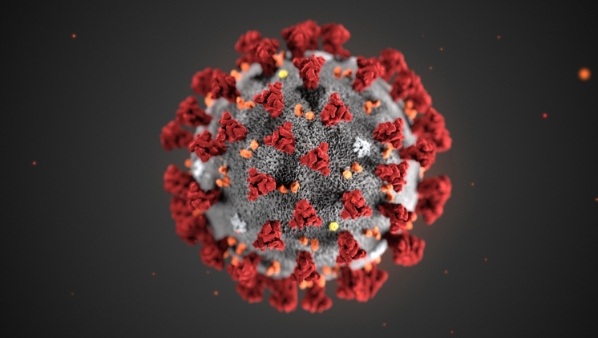
What is COVID-19?
Click for more infoWhat is COVID-19?
COVID-19 is a disease caused by a virus called severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2). It has caused more than 97 million infections and over 1 million deaths in the United States (https://covid19.who.int/region/amro/country/us). Almost 600 million infections and over 6 million deaths have occurred around the world (https://covid19.who.int). Some people with COVID-19 have mild symptoms, but others can become severely ill and die from the disease. Research is ongoing to uncover why certain individuals are more susceptible to severe illness and may die. . The majority of people with COVID-19 get better within weeks of illness, but some people experience post-COVID complications and conditions. Older people and those who have certain underlying medical conditions are more likely to get severely ill from COVID-19. Post-COVID conditions are characterized by a wide range of symptoms, including continued loss of taste and/or smell. People can begin to experience health problems any time from when they are first infected with SARS-CoV-2 to more than four weeks after first being infected.. COVID-19 vaccines are safe and very effective in preventing illness, hospitalization, and death. SARS-CoV-2 and its associated disease were reportedly unknown before the outbreak began in China in December 2019.
On February 11, 2020, the World Health Organization (WHO) announced an official name for the disease, abbreviated as COVID-19. ‘CO’ stands for ‘corona,’ ‘VI’ for ‘virus,’ and ‘D’ for disease. 19 is the year (2019) that cases of the virus were first reported in the world. On March 11, 2020, WHO declared the rapidly spreading novel coronavirus outbreak to be a global pandemic. The disease is now present in over 220 countries. Additionally, since it was first reported, several viral variants have emerged that are extremely contagious including the Delta and Omicron strains. Omicron and its subvariants, which are highly transmissible, have caused a dramatic increase in cases during the winters 2021-2023, causing disruptions across society. Recently, the US government warned that COVID-19 may keep surging in the winter months for years to come.
How does COVID-19 spread?
Click for more infoHow does COVID-19 spread?
COVID-19 spreads via respiratory transmission. when an infected person breathes out droplets and very small particles that contain the virus. These droplets and particles can be inhaled by other people or land on their eyes, nose, or mouth. In some circumstances, these droplets may contaminate surfaces. People who are closer than 6 feet from the infected person for more than 15 minutes are most likely to get infected. COVID-19 is spread in three main ways:
- Breathing in air when close to an infected person who is exhaling small droplets and particles that contain the virus.
- Having these small droplets and particles that contain virus land on the eyes, nose, or mouth, especially through splashes and sprays like a cough or sneeze.
- Touching eyes, nose, or mouth with hands that have the virus on them.
People who are asymptomatic (when the virus is detected but symptoms never develop) and people who are pre-symptomatic, (when the virus is detected before symptom onset), can both transmit the disease. Research suggests that as many as 40%-59% of cases in the United States may be asymptomatic. That means people can spread the disease without even knowing it.

Are booster shots available and recommended? Should I get one?
Click for more infoAre booster shots available and recommended? Should I get one?
The case for a booster shot:
Vaccines are the very best tool for preventing COVID-19. New CDC studies show that while all the COVID-19 vaccines authorized for use in the United States remain highly effective against preventing hospitalizations and deaths, the protection they provide against infection with the virus has weakened over the past several months, especially among certain populations including those people who aged 65 years and older and those who are immunocompromised. That is why bivalent booster shots are now recommended for all individuals. Breakthrough infections are rising among people who are fully vaccinated but the illness tends to be milder.
The recent emergence and rapid spread of the Omicron variants in the United States and around the world further emphasizes the importance of being fully vaccinated and getting booster shots to maximize protection against COVID-19. Studies have indicated a booster of Pfizer Inc.‘s vaccine provides a 25-fold increase in neutralizing antibodies that fight the variant, Moderna Inc.‘s booster produces a 37-fold increase in antibodies, and two doses of Johnson & Johnson‘s vaccine cut hospitalizations in South Africa by 85%. The bivalent boosters from Pfizer and Moderna, which are the current CDC-recommended shots, provide additional protection against novel variants as well as the older strains. (https://www.cdc.gov/mmwr/volumes/71/wr/mm7148e1.htm).
Evidence is still accruing regarding the duration of protection following vaccination. One model predicted that an initial vaccine effectiveness of 90% would likely decline to approximately 70% around 250 days post-vaccination. This model does not account for other factors that could contribute to susceptibility to the virus such as non-serologic components of the immune response or the impact of new circulating variants. Recent studies have demonstrated waning of both antibody titers and vaccine effectiveness against infection over time, especially among older and immunocompromised populations. Additional studies show that among healthcare and other frontline workers, vaccine effectiveness against COVID-19 infections has been decreasing likely due to the combination of reduced immune protection as time passes since getting vaccinated, as well as the greater infectiousness of the Omicron variants. A recent Israeli study found that immunity after a second booster declined by 4 weeks and was significantly diminished by 8 weeks . The decline in effectiveness against infection may result from waning vaccine immunity, a lapse in people taking precautions like wearing masks or the rise of the highly contagious Delta and Omicron variants, or a combination of all three. That’s why people who are eligible should get their booster shots now.
Booster Recommendation and Availability
Everyone ages 6 months and older can get a bivalent booster shot 2 months after completion of the primary vaccination series. Some people may prefer the vaccine type that they originally received whereas others may prefer to get a different booster. The CDC recommendations now allow for this type of mix and matching of vaccines for booster shots, except for children aged 6 months – 4 years.
Mixing & Matching Vaccines
The CDC has issued guidance that Americans who are eligible for boosters can receive a different COVID-19 vaccine than the one they initially were administered, except for children aged 6 months – 4 years. The CDC has released information about who might benefit from choosing one booster over another.
The reason for this mixing of vaccines recommendation includes data from a study showing that the antibody levels of those who had received a Johnson & Johnson vaccine followed by a Moderna booster rose 76-fold within 15 days, whereas the antibody levels of those who received a Johnson & Johnson booster rose only fourfold during the same period. A Pfizer booster raised antibody levels 35-fold in Johnson & Johnson recipients.
Additional Booster Shots
Immunocompromised Americans are eligible for additional boosters to protect them against COVID-19, according to recent recommendations from the Centers for Disease Control and Prevention (CDC). mRNA bivalent boosters are the recommended option for all individuals. Israel was the first to deliver a fourth vaccine dose for people most vulnerable to coronavirus including those over the age of 60 and immunocompromised individuals. A second and third booster dose of an mRNA COVID-19 vaccine is recommended for certain people who have a weakened immune system and people age 50 or older. The second booster dose can be given to those eligible 2 months after a first booster dose of any authorized or approved COVID-19 vaccine and the third booster can be given at least four months after the prior dose.
Booster Recommendation and Availability
Everyone ages 12 and older can get a booster shot. If you are 18 years or older you may choose which COVID-19 mRNA vaccine you receive as a booster. Some people may prefer the vaccine type that they originally received whereas others may prefer to get a different booster. The CDC recommendations now allow for this type of mix and match dosing for booster shots. To learn more about vaccine boosters, see below:
Pfizer-BioNTech Vaccine
COVID-19 Vaccine booster shots are currently recommended for all Pfizer-BioNTech vaccine recipients over the age of 12 who completed their initial two dose series at least 5 months ago. Anyone over the age of 18 who received another vaccine type, can get a Pfizer booster. For those people who are immunocompromised, a 2nd booster vaccine is recommended 4 months after receiving the 1st booster shot. These are people who have undergone solid organ transplantation, or who are living with conditions that are considered to have an equivalent level of immunocompromise. A second booster dose may be administered to individuals 50 years of age and older at least 4 months after receipt of a first booster dose of any authorized or approved COVID-19 vaccine.
Moderna Vaccine
COVID-19 Vaccine booster shots are currently available for Moderna vaccine recipients over the age of 18 who completed their initial series at least 5 months ago. All adults 18 years and older can choose to get their booster shot with the Moderna vaccine A second booster dose of the Moderna COVID-19 Vaccine may be administered at least 4 months after the first booster dose of any authorized or approved COVID-19 vaccine to individuals 18 years of age and older who are immunocompromisedA second booster dose may also be administered to individuals 50 years of age and older at least 4 months after receipt of a first booster dose of any authorized or approved COVID-19 vaccine.
Johnson and Johnson Vaccine
COVID-19 Vaccine booster shots are currently available for the following Johnson & Johnson recipients who were vaccinated at least 2 months ago. Adults who are 18 years and older who initially received a Johnson and Johnson vaccine can choose to get mRNA boosters with a Moderna or Pfizer vaccine.
Mixing & Matching Vaccines
The CDC has issued guidance that Americans who are eligible for boosters can receive a different COVID-19 vaccine than the one they initially were administered. The CDC has released information about who might benefit from choosing one booster over another.
The reason for this mixing of vaccines recommendation includes preliminary data from a recent study showing that the antibody levels of those who had received a Johnson & Johnson vaccine followed by a Moderna booster rose 76-fold within 15 days, whereas the antibody levels of those who received a Johnson & Johnson booster rose only fourfold during the same period. A Pfizer booster raised antibody levels 35-fold in Johnson & Johnson recipients.
Additional Booster Shots
Immunocompromised Americans are eligible for a fourth shot to protect them against COVID-19, according to recent recommendations from the Centers for Disease Control and Prevention (CDC). Israel was the first to deliver a fourth vaccine dose for people most vulnerable to coronavirus including those over the age of 60 and immunocompromised individuals. A second booster dose of an mRNA COVID-19 vaccine is recommended for certain people who have a weakened immune system and people age 50 or older. This second booster dose can be given to those eligible four to five months after a first booster dose of any authorized or approved COVID-19 vaccine.
When and where should I get a booster shot? What should I bring to the appointment?
Click for more infoWhen and where should I get a booster shot? What should I bring to the appointment?
Everyone ages 6 months and older should get a bivalent booster shot 2 months after they have completed their COVID-19 vaccine primary series. The CDC recommends the Pfizer or Moderna bivalent boosters regardless of the type of vaccine administered in a person’s primary vaccine series. (https://www.cdc.gov/coronavirus/2019-ncov/vaccines/stay-up-to-date.html).
To find a COVID-19 vaccine or booster, search vaccines.gov, text your ZIP code to 438829, or call 1-800-232-0233 to find locations near you. If you need help scheduling your booster shot, contact the location that set up your previous appointment. Read about others ways you can find a vaccine provider here if you need to get your booster shot in a location that is different from where you received your previous shot. When going to your booster appointment,, remember to bring your CDC COVID-19 Vaccination Record card so your provider can fill in the information about the date and type of your booster dose. If you did not receive a card at your first appointment, contact the vaccination site where you got your first shot or your state health department to find out how you can get a CDC card.
Be prepared to experience some side effects after getting a COVID-19 vaccine. These are normal signs that your body is building protection against COVID-19. Record the side effects that you experience in v-safe. If you enter your booster shot in your v-safe account, the system will send you daily health check-ins.
Be prepared to experience some side effects after getting a COVID-19 vaccine. These are normal signs that your body is building protection against COVID-19. Record the side effects you experience in v-safe. If you enter your booster shot in your v-safe account, the system will send you daily health check-ins.
How can I protect myself from COVID-19?
Click for more infoHow can I protect myself from COVID-19?
Getting vaccinated is the most important thing you can do to protect yourself from COVID-19.
If you are not vaccinated, the most effective public health measures to protect against the disease include:
- Learning about COVID-19 and how it could impact you, your family and community
- Making a decision to get vaccinated and getting a booster dose as soon as you are eligible
- Getting tested to know whether you have the disease and to prevent its spread to other people
- Wearing high quality masks
- Social distancing at least 6 feet apart from others
- Avoiding crowded and poorly ventilated spaces
- Washing your hands often for at least 20 seconds
- Disinfecting surfaces routinely
- Covering your coughs and sneezes
- Monitoring your health daily
- Getting tested if you’ve been exposed or are will be an indoor group gathering
- Staying at home if you have been exposed to the virus and are not vaccinated
- Following local and state guidelines
Refer to the CDC Website for more information.

Who is most at risk for experiencing severe illness?
Click for more infoWho is most at risk for experiencing severe illness?
There is currently a surge in U.S. coronavirus infections fueled by the highly contagious Omicron and its emerging subvariants. 20% of Americans are currently unvaccinated. That’s why getting vaccinated and boosted and taking preventive measures against COVID-19 such as wearing a mask and following other public health guidance is so important, especially if you or someone you are close to belong to one of the high-risk groups described below.
These people are more likely than others to become severely ill with COVID-19 including seniors and people with underlying medical conditions. Severe illness means that a person with COVID-19 may require hospitalization, intensive care, a ventilator to help them breathe, or that they may even die. People of any age with the following health conditions are at increased risk of severe illness from COVID-19:
-
- Cancer
- Chronic kidney disease
- Chronic lung diseases including COPD, asthma, interstitial lung disease, cystic fibrosis, and pulmonary hypertension
- Dementia or other neurological conditions
- Diabetes (type 1 or type 2)
- Down’s Syndrome
- Immunocompromised state (weakened immune system)
- Mental Illness and/or Substance Use Disorders
- Overweight and Obesity (body mass index [BMI] of 30 or higher)
- Heart conditions including heart failure, coronary artery disease, cardiomyopathies, or hypertension
- HIV infection
- Liver Disease
- Sickle cell disease or thalassemia
- Smoking, current and former
- Solid or blood stem transplant
- Stroke or cerebrovascular disease
- Tuberculosis
Racial and Ethnic Disparities – People of color have been disproportionately impacted by COVID-19. Long-standing systemic health and social inequities have put many racial and ethnic minority groups at increased risk of getting sick and dying from COVID-19. As compared to non-Hispanic Whites, at the beginning of the pandemic, Black and Hispanics are estimated to be twice as likely to be infected with COVID-19, and more than twice as likely to die from the disease. Click here to view COVID-19 racial/ethnic data in the United States.
Pregnancy – pregnant people, and those who have recently given birth, are at a higher risk for severe illness from COVID-19 when compared to non-pregnant people. They are eligible and encouraged to receive COVID-19 vaccines to prevent the disease. Physiological changes that occur in the body during pregnancy that increase risk for severe illness from respiratory viral infections like COVID-19 can persist after pregnancy. For example, increased risk for developing blood clots during pregnancy can continue after delivery and increase the risk for severe illness. Studies have shown that pregnant people with COVID-19 are also at increased risk for preterm birth (delivering the baby earlier than 37 weeks) and other poor pregnancy outcomes such as miscarriage. If you have COVID-19 and have just given birth, learn more about caring for your baby and breast feeding here.(https://jamanetwork.com/journals/jama/fullarticle/2788985)
Recent studies have shown that women who breastfeed can pass immunity to COVID-19 to their infant.
If you are pregnant and have questions about COVID-19 vaccines
Pregnant and recently pregnant and breastfeeding people can receive a COVID-19 vaccine. If you would like to speak to someone about COVID-19 vaccination during pregnancy, you might want to contact MotherToBaby. MotherToBaby experts are available to answer questions in English or Spanish by phone or chat. This free and confidential service is available Monday–Friday from 8am–5pm (local time). To reach MotherToBaby:
-
-
- Call 1-866-626-6847
- Chat live or send an email MotherToBaby – click here
-
Racial and Ethnic Disparities – People of color have been disproportionately impacted by COVID-19. Long-standing systemic health and social inequities have put many racial and ethnic minority groups at increased risk of getting sick and dying from COVID-19. As compared to non-Hispanic Whites, Black and Hispanics are estimated to be twice as likely to be infected with COVID-19, and more than twice as likely to die from the disease. Click here to view COVID-19 racial/ethnic data in the United States.
Pregnancy – pregnant people, and those who have recently given birth, are at a higher risk for severe illness from COVID-19 when compared to non-pregnant people. They can receive a COVID-19 vaccine to prevent the disease. Physiological changes that occur in the body during pregnancy that increase risk for severe illness from respiratory viral infections like COVID-19 can persist after pregnancy. For example, increased risk for developing blood clots during pregnancy can continue after delivery and increase the risk for severe illness. Studies have shown that pregnant people with COVID-19 are also at increased risk for preterm birth (delivering the baby earlier than 37 weeks) and other poor pregnancy outcomes such as miscarriage. If you have COVID-19 and have just given birth, learn more about caring for your baby and breast feeding here.
Recent studies have shown that women who breastfeed can pass immunity to COVID-19 to their infant.
If you are pregnant and have questions about COVID-19 vaccines
Pregnant and recently pregnant and breastfeeding people can receive a COVID-19 vaccine. If you would like to speak to someone about COVID-19 vaccination during pregnancy, please contact MotherToBaby. MotherToBaby experts are available to answer questions in English or Spanish by phone or chat. This free and confidential service is available Monday–Friday from 8am–5pm (local time). To reach MotherToBaby:
-
-
- Call 1-866-626-6847
- Chat live or send an email MotherToBaby – click here
-

What is known about the new SARS-CoV2 variants that have emerged?
Click for more infoWhat is known about the new SARS-CoV2 variants that have emerged?
Several variants of the SARS-CoV-2 virus that causes COVID-19 have been documented in the United States and globally during the pandemic. The Delta variant represented the dominant strain in America and worldwide until December 2021. However, by January 2022, 95% of new infections in the United States were with the highly contagious Omicron variant, first reported in South Africa in December 2021. According to the CDC, cases due to the Omicron variant surged during the winter of 2022, as the overall national vaccination rate plateaued. In early April, 2022, the highly contagious Omicron subvariant known as BA.2, led to a surge of coronavirus cases in Europe, became the dominant strain of new cases of the virus reported in the United States. Another Omicron subvariant, XBB.1.5, called the “kraken” strain, has recently emerged and is extremely transmissible, very drug-resistant, and significantly immune system evading. According to the WHO, it is circulating in at least 38 countries with the highest prevalence in the United States where it accounts for 46% of cases and 74% of cases in Northeastern states. It is rapidly spreading across the world and will likely become the next dominant subvariant. Some studies show lackluster performance of the bivalent vaccine against this variant while other research find the bivalent to be more effective than the monovalent vaccine but neither booster provides adequate protection. Alarmingly, the Omicron variant is highly transmissible and its subvariants BA.2 and XBB1.5 are 3-5 times more transmissible than the original omicron variant. An increasing number of breakthrough cases have been reported in vaccinated people.
Booster shots are now recommended in America by the CDC for all people over the age of 6 months.. The mRNA bivalent boosters incorporate elements of emerging variants, providing broad protection against them. The CDC also recommends a 2nd booster for people ages 12 and older who are moderately or severely immunocompromised 5 months after their 1st booster. A second booster dose is also recommended for those people over the age of 50 in the United States. A third bivalent booster is recommended for immunocompromised individuals and those over 50. Learn more about the COVID-19 variants here and below:
- The Omicron Variant (B.1.1.529): It is unknown where the variant originated although it was detected first in the southern region of Africa. Some experts have described it as the “worst strain ever”—as contagious as measles– as it has all the mutations of previous variants with additional ones that made it more transmissible and somewhat less responsive to vaccines. The variant carries 32 mutations on the spike protein, and more than 50 in total, the most ever recorded and twice as many as the previously dominant Delta strain. Studies reveal that the new variant is highly transmissible but its effects on hospitalization and deaths rates as well as its response to currently available vaccines is still being determined. Breakthrough infections in people who are fully vaccinated have been observed, but vaccines are effective at preventing severe illness, hospitalizations, and death. Research has revealed that fully vaccinated people who become infected with the Omicron variant and subvariant BA.2 can spread the virus to others. All FDA-approved or authorized vaccines were reported to be effective against severe illness, hospitalizations, and deaths from the Omicron variant. The emergence of the Omicron variant further emphasized the importance of people getting vaccinated and receiving boosters to gain protection against this disease.
- The “Stealth” Omicron Variant (BA.2): In April 2022, reports from the CDC showed that BA.2 is was the dominant version of the virus in new cases in the United States. Studies from Britain suggest this strain’s growth rate is 80 percent faster than the original omicron variant. Fortunately, it does not appear to cause more severe disease as compared to the original omicron strain. Additionally, BA.2 is not significantly different from BA.1 except that it appears to be 2-3 times more transmissible. People who were previously infected with omicron are unlikely to be reinfected with the BA.2 variant. A recent study from Denmark (not yet published) found only 47 instances of BA.2 reinfection following infection with the original omicron strain, out of more than 1.8 million cases of COVID-19 that were reported. On a population level, the combination of recovery from omicron infection and vaccination means that the United States has a high rate of immunity against BA.2 in many areas of the country.
“Kraken” Omicron Variant (XBB1.5): A new Omicron subvariant, XBB1.5 (nicknamed “Kraken”) emerged in late 2022 and continues to rise in 2023. Research to understand Kraken’s rise and features is still ongoing, but the WHO has called XBB1.5 the most transmissible strain so far. Of note, all currently available monoclonal antibodies are deemed to be ineffective against XBB.1.5. Antiviral medications such as Paxlovid and remdesivir may be considered for the treatment of eligible infected patients at high risk of progressing to severe disease. (https://www.yalemedicine.org/news/omicron-xbb-kraken-subvariant)
- The Lambda Variant (C.37): First detected in Peru in August 2020, it spread throughout that country in 2021, accounting for the majority of new cases in that period. At least 29 other countries have reported Lambda variant COVID-19 infections. Chile, Argentina, and Ecuador have seen the most significant increases outside of Peru, and the WHO designated it a “variant of interest” on June 14, 2021. Researchers in Japan have found that the lambda variant may be more resistant to vaccines. Their study suggests that three mutations in the lambda variant’s spike proteins make it more resistant to antibodies induced by vaccination and two additional mutations make it more infectious. Its mutations have suspected implications, such as potential increased transmissibility or possible increased resistance to neutralizing antibodies, according to the WHO. To date, the Lambda variant is not as concerning to experts as the highly transmissible Omicron and Delta variants.
- The Beta Variant (B.1.351): Since being identified in South Africa in early October 2020, this variant has been reported in more than eighty countries including the United States, Canada, Australia and Israel. On January 28, 2021, South Carolina officials reported that two people with this variant had no travel history, indicating the first instances of this strain identified in America. This variant shares some similarities with the alpha variant and, like that strain, appears to be more transmissible. But there is no evidence that it is more lethal than other strains. South Africa stopped offering the AstraZeneca-Oxford vaccine (which is not available in the U.S.) early in 2021 after clinical trials showed it did not provide strong protection against mild and moderate disease from the Beta variant. Pfizer-BioNTech, Moderna, and Johnson & Johnson also reported less protection with their vaccines against the Beta variant
- The Gamma Variant (P.1): Sequencing studies revealed this variant was circulating in Brazil in July 2021. Since then, it has also been reported in Peru, Germany, South Korea and Japan, among other nations. On January 25, 2021, Minnesota health officials confirmed the first U.S. case of Gamma variant in a resident with a recent travel history to Brazil. Researchers believe this variant is more transmissible than the original strain, and there is also evidence that antibodies might not recognize the P. 1 variant, which could lead to possible reinfection. Scientific evidence suggests that today’s vaccines work against this variant first identified in Brazil.
- The Alpha Variant (B.1.1.7): First reported in the United Kingdom, hundreds of countries, including the United States, have seen many cases of COVID-19 linked to this variant of the virus. The variant first identified in the U.K. is more transmissible than the original strain. Scientists agree that vaccines are effective against this particular variant which is no longer prevalent in the United States.
The CDC in collaboration with other public health agencies and private sector labs is working to detect and characterize emerging viral variants. While the US initially ranked 43rd in the world for genomic testing early in the pandemic, it now ranks 20th in conducting genomic tests to track new viral variants. This information is important for understanding how the virus is spreading as well for determining how effective currently available vaccines are against them and whether additional boosters will be needed in the future.
ADDITIONAL INFORMATION :
- New COVID-19 Variants
- National Genomic Dashboard
- What is Genomic Surveillance?
- Emerging SARS-CoV-2 Variants
- SARS-CoV-2 Variants
- New York Times’ Variants Tracker
- The Lambda Variant (C.37): First detected in Peru in August 2020, spreading there in 2021 and accounted for the majority of new cases there. At least 29 other countries have reported Lambda variant COVID-19 infections over the past months. Chile, Argentina, and Ecuador have seen the most significant increases outside of Peru, and the WHO designated it a “variant of interest” on June 14, 2021. Preliminary data suggests the effectiveness of mRNA vaccines against this variant, although these findings have not yet been peer reviewed. Researchers in Japan have found that the lambda variant may be more resistant to vaccines. While their study has yet to be peer reviewed, it suggests that three mutations in the lambda variant’s spike proteins make it more resistant to antibodies induced by vaccination and two additional mutations make it more infectious. Its mutations have suspected implications, such as potential increased transmissibility or possible increased resistance to neutralizing antibodies, according to the WHO. To date, the Lambda variant is not as concerning to experts as the highly transmissible Omicron and Delta variants.
- The Beta Variant (B.1.351): Since being identified in South Africa in early October 2020, this variant has been reported in more than eighty countries including the United States, Canada, Australia and Israel. On January 28, 2021, South Carolina officials reported that two people with this variant had no travel history, indicating the first instances of this strain identified in America. This variant shares some similarities with the alpha variant and, like that strain, appears to be more transmissible. But there is no evidence that it is more lethal than other strains. South Africa stopped offering the AstraZeneca-Oxford vaccine (which is not available in the U.S.) early in 2021 after clinical trials showed it did not provide strong protection against mild and moderate disease from the Beta variant. Pfizer-BioNTech, Moderna, and Johnson & Johnson also reported less protection with their vaccines against the Beta variant
- The Gamma Variant (P.1): Sequencing studies revealed this variant was circulating in Brazil in July 2021. Since then, it has also been reported in Peru, Germany, South Korea and Japan, among other nations. On January 25, 2021, Minnesota health officials confirmed the first U.S. case of Gamma variant in a resident with a recent travel history to Brazil. Researchers believe this variant is more transmissible than the original strain, and there is also evidence that antibodies might not recognize the P. 1 variant, which could lead to possible reinfection. Scientific evidence suggests that today’s vaccines work against this variant first identified in Brazil.
- The Alpha Variant (B.1.1.7): First reported in the United Kingdom, hundreds of countries, including the United States, have seen many cases of COVID-19 linked to this variant of the virus. The variant first identified in the U.K. is more transmissible than the original strain. Scientists agree that vaccines are effective against this particular variant which is no longer prevalent in the United States.
The CDC in collaboration with other public health agencies and private sector labs is working to detect and characterize emerging viral variants. While the US initially ranked 43rd in the world for genomic testing early in the pandemic, it now ranks 20th in conducting genomic tests to track new viral variants. This information is important for understanding how the virus is spreading as well for determining how effective currently available vaccines are against them and whether additional boosters will be needed in the future.
ADDITIONAL INFORMATION :
- New COVID-19 Variants
- National Genomic Dashboard
- What is Genomic Surveillance?
- Emerging SARS-CoV-2 Variants
- SARS-CoV-2 Variants
- New York Times’ Variants Tracker
How do the recently detected variants affect the course of the disease?
Click for more infoHow do the recently detected variants affect the course of the disease?
Multiple variants of the virus that causes COVID-19 are circulating in the United States. The dominant variants, especially Omicron and Delta, appear to spread more easily and rapidly than other variants, leading to increased numbers of COVID-19 cases. The Omicron variant now representing more than 95% of new infections in the United States has led to a record high level of COVID cases around the world. The Omicron subvariant BA.2 was responsible for more than 51% of new infections in America in spring and summer 2022. Another highly transmissible subvariant XBB.1.5 that has recently emerged is responsible for 49% of new infections in America and 84% of cases in the New England area as of early 2023.
Scientists are studying COVID-19 variants to learn more about how to control their spread. They want to understand whether the variants:
- Spread more easily from person-to-person
- Cause more severe disease in people
- Are detected by currently available viral tests
- espond to medicines currently being used to treat people for COVID-19
- Change the effectiveness of COVID-19 vaccines
To date, studies suggest that currently available vaccines in the United States protect against severe disease caused by these variants. This is being closely investigated and more studies are underway. However, a rise in breakthrough infections in fully vaccinated people and studies conducted by Pfizer and the government of Israel suggest a decrease in vaccine effectiveness although protection is still significant in preventing hospitalizations and death. However, booster shots are now recommended five months after being fully vaccinated with mRNA vaccines and two months after receiving the Johnson and Johnson vaccine. Two additional boosters have been recommended for some population groups. More studies are needed including genomic sequencing of breakthrough infections in fully vaccinated people to better understand who is most at risk and whether additional booster vaccines will be needed in the future.
Rigorous compliance with public health mitigation strategies, such as vaccination, physical distancing, use of effective masks, hand hygiene, and isolation and quarantine of infected individuals, is essential to limit the spread of the virus that causes COVID-19 and to protect the health of the public.
To date, studies suggest that currently available vaccines in the United States protect against severe disease caused by these variants. This is being closely investigated and more studies are underway. However, a rise in breakthrough infections in fully vaccinated people and studies conducted by Pfizer and the government of Israel suggest a decrease in vaccine effectiveness although protection is still high to prevent hospitalizations and death. However, booster shots are now recommended five months after being fully vaccinated with mRNA vaccines and two months after receiving the Johnson and Johnson vaccine. More studies are needed including genomic sequencing of breakthrough infections in fully vaccinated people to better understand who is most at risk and whether additional booster vaccines will be needed in the future.
Rigorous compliance with public health mitigation strategies, such as vaccination, physical distancing, use of effective masks, hand hygiene, and isolation and quarantine of infected individuals, is essential to limit the spread of the virus that causes COVID-19 and to protect the health of the public.
ADDITIONAL RESOURCES
How effective are vaccines against the COVID-19 Delta variant?
Click for more infoHow effective are vaccines against the COVID-19 Delta variant?
According to the CDC, the Pfizer, Moderna, Novavax, and Johnson & Johnson vaccines offer significant protection against the Delta and Omicron variants. The bivalent mRNA boosters are recommended for all, regardless of the primary vaccination series, to provide broad protection against emerging variants. Most cases in the United States linked to the Delta and Omicron variants are occurring in unvaccinated people, though recent studies suggest that there is a significant rise in breakthrough infections in vaccinated individuals. Additionally, many Americans have not received their booster shots. Vaccination helps to protect against serious illness, hospitalization and death. Studies are underway to determine the ongoing effectiveness of currently available vaccines against emerging variants of the virus that causes COVID-19.
Although COVID-19 vaccines remain effective in preventing severe disease, studies suggest their effectiveness at preventing infection or severe illness wanes over time, especially in people ages 65 years and older. A recent study conducted in the United Kingdom found that the Pfizer-BioNTech vaccine was only 36% effective against the Delta variant after one dose, but 88% effective after two doses. New data from Israel suggests reduced efficacy of the Pfizer vaccine. After two immunizations, the vaccine was 39% effective at reducing the risk of infection, 40% effective at reducing the risk of symptomatic disease, but importantly was still 91% effective at preventing severe illness, hospitalization and death during a period when the Delta variant was the dominant strain in Israel. A study in Canada found that two doses of the Pfizer-BioNTech vaccine were 87% effective in protecting against symptomatic infection. The data suggests that mRNA vaccines like Pfizer and Moderna offer a high degree of protection against COVID-19 infection especially preventing severe illness, hospitalization and death.
Studies of Johnson & Johnson’s single shot COVID-19 vaccine had suggested it provides important protection; however, protection wanes after two months. Consequently, the CDC recommends that people get a booster shot of either the Pfizer or Moderna mRNA vaccines two months after receiving the Johnson & Johnson immunization. A study from South Africa found the Johnson & Johnson’s coronavirus vaccine helps prevent severe disease among those infected with the Delta variant, with the evidence showing that the single-dose shot was 71% effective against hospitalization and as much as 96% effective against death. A second and third mRNA booster following the initial J and J vaccine are recommended for specific populations groups.
As COVID-19 infections continue to spread, it is important to keep practicing the 3 W’s (wear a mask if you are unvaccinated and, in some settings, if you are vaccinated following state and local guidance; wash your hands; and watch your distance if unvaccinated) to prevent the spread of the virus.
Studies of Johnson & Johnson’s single shot COVID-19 vaccine had suggested it provides important protection; however, protection wanes after two months. The CDC recommends that people get a booster shot of either the Pfizer or Moderna mRNA vaccines two months after receiving the Johnson & Johnson immunization. A study from South Africa found the Johnson & Johnson’s coronavirus vaccine helps prevent severe disease among those infected with the Delta variant, with the evidence showing that the single-dose shot was 71% effective against hospitalization and as much as 96% effective against death.
However, other research which has not yet been peer reviewed found that the Johnson & Johnson vaccine may not be as effective at preventing illness caused by the Omicron, Delta and Lambda variants indicating that those who have received this immunization, should get a booster shot with one of the mRNA vaccines.
As COVID-19 infections continue to spread, it is important to keep practicing the 3 W’s (wear a mask if you are unvaccinated and in some settings if you are vaccinated following state and local guidance; wash your hands; and watch your distance if unvaccinated) to prevent the spread of the virus.
Can I get COVID-19 after being vaccinated?
Click for more infoCan I get COVID-19 after being vaccinated?
A small percentage of people who are fully vaccinated and boosted may still get infected with COVID-19 if they are exposed to the virus. These are called “vaccine breakthrough cases.” When these infections do occur among vaccinated people, they tend to be milder although some hospitalizations and deaths have been reported. We do not know for certain how often these breakthrough cases are occurring: since May 2021, the CDC has focused on investigating only hospitalized or fatal Covid-19 cases among people who have been fully vaccinated and have not required states to report all other breakthrough infections.
To prevent breakthrough infections, get booster shots when you are eligible. And if you live in an area with high transmission of COVID-19, you – as well as your family and community – will be better protected if you wear a mask when you are in indoor public places even if you are fully vaccinated. Be aware that even people who get asymptomatic or mild vaccine breakthrough infections can still be contagious
Additional Resources
What treatment options are currently available?
Click for more infoWhat treatment options are currently available?
Most people who become infected with COVID-19 have mild symptoms and can recover safely at home. Over-the-counter medicines such as acetaminophen (Tylenol) can treat many people’s symptoms. Consult your healthcare provider if you feel sick.
Currently, there is no cure for COVID-19. Several treatments are now available to be used at home or in outpatient and hospital settings. Scientists are studying a wide range of potential therapeutic interventions and approaches to treat COVID-19.
Anti-Viral At-Home Medications: In December 2021, the FDA authorized two medications in that are the first COVID-19 therapies that can be used at home and don’t require infusions or injections delivered by health professionals. Pfizer’s Paxlovid and Merck’s molnupiravir can both be taken at home to treat COVID-19 and should be started soon after symptoms develop. Paxlovid can be used by anyone 12 years and older who faces the highest risk of hospitalization, especially older people and those with other health conditions like heart disease, cancer or diabetes that make them more vulnerable to COVID-19. Molnupiravir is for adults with a positive COVID-19 test, early symptoms and who face a high risk of hospitalization. Molnupiravir carries a warning against use during pregnancy because it has the potential to cause birth defects. The FDA also issued guidance that molnupiravir should be considered only when other treatments are unavailable or otherwise inappropriate for a patient given its side effects and interactions with many other medications. Thus, Paxlovid, has become the first choice for at-home treatment of COVID-19, because of its superior benefits and milder side effects.
While these treatments are convenient, they come with a few caveats: the pills must be taken as soon as possible within five days of symptoms appearing. That means that you need to get tested, get a prescription and start the medication in a short window of time for it to be effective.
Other Antiviral Drugs. Remdesivir was the first FDA approved drug for treatment of COVID-19 in adult and pediatric patients, 12 years of age and older on May 1, 2021 for use in the hospital. The FDA recently approved its use for COVID-19 outpatients at high risk of being hospitalized as well. This decision provides a new treatment option for health care providers who want to keep COVID-19 patients out of the hospital when waves of infections are overwhelming medical facilities.
Dexamethasone. Research studies have found that dexamethasone, an inexpensive and widely used steroid, can reduce COVID-19 deaths in the severely ill by up to one third. The NIH recommends that this medication be used in hospitalized patients who require supplemental oxygen. NIH recommends against the use of dexamethasone or other systemic glucocorticoids to treat outpatients with mild to moderate COVID-19 who do not require hospitalization or supplemental oxygen.
Monoclonal Antibody (mAb) Treatments: During the pandemic, the FDA issued Emergency Use Authorization (EUA) for four investigational mAb treatments including Evushield that could attach to SARS-CoV-2, the coronavirus that causes COVID-19. These antibodies helped people’s immune systems recognize and respond more effectively to the virus. They were initially authorized for patients with mild to moderate COVID-19 cases including people who have had symptoms for 10 days or less, who are 12 years of age and older, and who are at high risk for progressing to serious COVID-19 and are not in the hospital.
However, as different strains of COVID-19 emerged, these monoclonal antibodies no longer work and have been removed from clinical use in all states.
I
Convalescent Plasma. Convalescent plasma was initially authorized by the FDA in August 2020, despite a lack of randomized trial data at the time, and in February 2021, it was scaled back to only to the use of high-titer plasmafor hospitalized patients early in their disease course who could not mount a sufficient immune response to COVID infection. Recently, FDA began allowing the therapy in the outpatient setting, but still limited treatment to those who are immunocompromised. The Convalescent Plasma Benefit Index Calculator allows doctors to input certain patient criteria to determine if their patient may benefit from convalescent plasma (age, oxygen need, blood type, and history of either diabetes, heart disease, or pulmonary disease). The meta-analysis and study on the validated treatment benefit index (TBI) tool derived from it were both published in JAMA Network Open. Many studies have been conducted on convalescent plasma some with positive and others with negative findings on its effectiveness in treating COVID-19.
Other substances. Do NOT take non-pharmaceutical chloroquine phosphate or ingest or inject any disinfectants. Do NOT take medication to treat coronavirus that has not been prescribed by your healthcare provider for this explicit purpose. Do NOT take ivermectin to treat COVID-19. It is not effective as a therapy and can have serious side effects. Read the research here.
More Information on COVID-19 Treatments
Refer to the NIH’s COVID-19 Treatment Guidelines to stay up-to-date on information regarding therapies for COVID-19.
Visit the New York Times’ treatment tracker here for helpful information.
Other Antiviral Drugs. Remdesivir was the first FDA approved drug for treatment of COVID-19 in adult and pediatric patients, 12 years of age and older on May 1, 2021. The FDA recently approved its use for COVID-19 outpatients at high risk of being hospitalized as well. This decision provides a new treatment option for health care providers who want to keep COVID-19 patients out of the hospital when waves of infections are overwhelming medical facilities.
Dexamethasone. Research studies have found that dexamethasone, an inexpensive and widely used steroid, can reduce COVID-19 deaths in the severely ill by up to one third. The NIH recommends that this medication be used in hospitalized patients who require supplemental oxygen. The NIH recommends against the use of dexamethasone or other systemic glucocorticoids to treat outpatients with mild to moderate COVID-19 who do not require hospitalization or supplemental oxygen.
Monoclonal Antibody (mAb) Treatments: During the pandemic, the FDA issued Emergency Use Authorization (EUA) for four investigational mAb treatments that could attach to SARS-CoV-2, the coronavirus that causes COVID-19. These antibodies helped people’s immune systems recognize and respond more effectively to the virus. They were initially authorized for patients with mild to moderate COVID-19 cases including people who have had symptoms for 10 days or less, who are 12 years of age and older, and who are at high risk for progressing to serious COVID-19 and are not in the hospital. However, as different strains of COVID-19 emerged, these antibodies no longer work and have been removed from clinical use in all states.
In recent weeks, as the Omicron variant and subvariant BA.2 have become dominant in communities across the country, only sotrovimab was recommended for use against this strain; the other two mAbs produced by Regeneron and Eli Lilly have not been found to be effective against the omicron variant. However, with the dominance of omicron and the BA.2 strain, sotrovimab is no longer effective against it and has been removed from clinical use in the United States.
Convalescent Plasma. Convalescent plasma was initially authorized by the FDA in August 2020, despite a lack of randomized trial data, and in February 2021, it was scaled back to only high-titer plasma for hospitalized patients early in their disease course who could not mount a sufficient immune response to COVID infection. Recently, FDA began allowing the therapy in the outpatient setting, but still limited treatment to those who are immunocompromised. The Convalescent Plasma Benefit Index Calculator allows doctors to input certain patient criteria to determine if their patient may benefit from convalescent plasma (age, oxygen need, blood type, and history of either diabetes, heart disease, or pulmonary disease). The meta-analysis and study on the validated treatment benefit index (TBI) tool derived from it were both published in JAMA Network Open.
Other substances. Do NOT take non-pharmaceutical chloroquine phosphate or ingest or inject any disinfectants. Do NOT take medication to treat coronavirus that has not been prescribed by your healthcare provider for this explicit purpose. Do NOT take ivermectin to treat COVID-19. It is not effective as a therapy and can have serious side effects. Read the research here.
More Information on COVID-19 Treatments
Refer to the NIH’s COVID-19 Treatment Guidelines to stay up-to-date on information regarding therapies for COVID-19.
Visit the New York Times’ treatment tracker here for helpful information.

Is it safe to travel?
Click for more infoIs it safe to travel?
The CDC recommends delaying travel until you are up-to-date with your COVID-19 vaccines. If you are not up to date with your COVID-19 vaccines and must travel, get tested both before and after your trip. People who are fully vaccinated with an FDA-authorized vaccine or a vaccine authorized for emergency use by the World Health Organization can travel safely within the United States.
During travel, wearing a mask over your nose and mouth is recommended but no longer required on planes, buses, trains, and other forms of public transportation traveling into, within, or out of the United States and while indoors at U.S. transportation hubs such as airports and stations.
After travel, be sure to monitor for COVID-19 symptoms; isolate and get tested if you develop symptoms. If you are up to-date on your vaccines and boosers, you do NOT need to get tested or self-quarantine after traveling.
If you are not fully vaccinated and must travel, it’s suggested that you take the following steps to protect yourself and others from COVID-19, Consider getting a viral test 1-3 days before your trip. While you are traveling, keep practicing the 3 W’s (wear a high-quality mask if you are unvaccinated and in some settings if you are vaccinated; wash your hands; and watch your distance). After you travel, get a viral test 3-5 days after travel and self-monitor for COVID-19 symptoms. If you develop symptoms, isolate and get tested. Follow all state and local recommendations and requirements.
After traveling, to be safe, you might consider getting tested 3-5 days following your return, self-monitor for COVID-19 symptoms; or if you develop symptoms, and follow all state and local guidance after returning to the United States.
People who are not up-to-date on their vaccinations should get tested 1-3 days before domestic traveling, as well as get tested again 3-5 days after completing travel.
When traveling internationally, each country has its own guidance and requirements for testing, vaccinations and self-quarantine upon arrival or if you get sick. Over the past months, many countries have removed strict COVID requirements that were in place, Therefore, it is very important to be knowledgeable about the requirements BEFORE you travel. To learn more about the steps to take to travel safely, visit this link.
After traveling, get tested 3-5 days following your return, self-monitor for COVID-19 symptoms; isolate and get tested if you develop symptoms, and follow all state and local guidance after returning to the United States.
People who are not up-to-date on their vaccinations should get tested 1-3 days before domestic traveling, as well as get tested again 3-5 days after completing travel. They must also self-quarantine for a full 5 days after travel, even if after a negative test.
When traveling internationally, each country has its own guidance and requirements for testing, vaccination and self-quarantine. Therefore, it is very important to be knowledgeable about the requirements BEFORE you travel. To learn more about the steps to take to travel safely, visit this link.

How does the pandemic end?
Click for more infoHow does the pandemic end?
At some point in the future, the World Health Organization will determine when enough countries have reduced their COVID-19 cases sufficiently — or at the minimum, hospitalizations and deaths — to declare the pandemic officially over. Exactly what that threshold will be isn’t clear at this time. Experts are warning that COVID may be here to stay and that we will have surges during the winter months for years to come.
A beginning of the end of the coronavirus pandemic could be on the horizon if at least 80-90% of people in our country were fully vaccinated and boosted, but the timeline for actually getting there feels like it shifts daily given recent surges in infections in the United States and worldwide with the highly contagious Omicron and Delta variants. Also, with 20% of individuals in the United States still unvaccinated, many infections are still occurring, fueling the pandemic. Furthermore, with hundreds of millions of unvaccinated people worldwide, there are many opportunities for new variants to emerge and spread globally.
Looking forward, there are several possible ways for the COVID-19 pandemic to end:
- Vaccines. Vaccinating 80-90% of the population is a critical component of ending the pandemic. Efforts to develop and deploy safe and effective vaccines in record time are underway around the world but currently face many hurdles, such as mass production and distribution, the durability of their effectiveness, as well as vaccine hesitancy. Furthermore, scientists are still investigating whether someone who has been sick with COVID-19 and has developed antibodies has enduring protection or can become reinfected. If reinfection is possible as has been observed with the recent rise in breakthrough infections, it could present complications for a successful vaccine as do the many variant strains that are circulating around the world. Recent research reveals that people need booster vaccines to protect against new contagious variants of the virus circulating in communities. Current studies are evaluating how often boosters may be needed to maintain immunity against COVID-19.
- Treatments. A variety of treatments have become available, and others are being explored to alleviate severe illness and reduce mortality rates. Some of these options include medications to use at home, antivirals treatments, steroids, and immune modulators. However, some treatments are no longer effective against the new Omicron subvariants. If a range of effective treatments become widely available and easy to use at home, this could help curtail the devastating toll of COVID-19.
- Herd Immunity. When approximately 80-90% of the population has been infected or immunized, ‘herd immunity’ will hinder viral spread to help end the pandemic. However, this could take years, and with reinfection of COVID-19 occurring and very contagious viral variants reducing vaccine effectiveness as well as with many unvaccinated people in America and around the world, herd immunity may not be readily achieved. Some experts believe that the intense spike of cases amid the omicron wave will help lead to a significant amount of natural immunity, adding to the vaccine immunity across the U.S. and in many countries. However, it is still unclear how long this immunity will last and whether current vaccines can fully protect against the new subvariants that are emerging.
- We learn to live with it. In this scenario, instead of “beating the virus,” people adjust their lifestyles to learn to live with the disease. Experts hypothesize that this happens when the virus is controlled in such a way that it does not disrupt society, the economy, or health systems. In the United States and many other areas of the world, there has been a relaxing of masking and other guidelines in communities where there are lower rates of infections. Many experts now believe that COVID-19 may become endemic like the flu but might periodically cause outbreaks in the winter such as happens with influenza. Additionally, if mutant strains continue emerging, spreading, and become resistant to current vaccines, then more booster vaccines will be needed as is the case for immunizing against influenza. Additionally, other vaccine types such as intranasal formulations or a universal coronavirus vaccine should be explored that could provide more durable immunity. The virus might continue to cause mild illness for some and more serious illness for others, depending on their overall health, vaccine status and prior infections. But in this scenario, society is open and people are working, attending school and social events.
- Herd Immunity. When approximately 80-90% of the population has been infected or immunized, ‘herd immunity’ will hinder viral spread to help end the pandemic. However, this could take years, and with reinfection of COVID-19 occurring and very contagious viral variants reducing vaccine effectiveness as well as with many unvaccinated people in America and around the world, herd immunity may not be readily achieved. Some experts believe that the intense spike of cases amid the omicron wave will help lead to a significant amount of natural immunity, adding to vaccine immunity across the U.S. and in many countries. However, it is still unclear how long this immunity will last.
- We learn to live with it. In this scenario, instead of “beating the virus,” people adjust their lifestyles to learn to live with the disease. Experts hypothesize that this happens when the virus is controlled in such a way that it does not disrupt society, the economy, or health systems. In the United States, in recent weeks, there has been a relaxing of masking and other guidelines in communities where there are lower rates of infections. Many experts believe that COVID-19 may become endemic like the flu but might periodically cause outbreaks such as happens with influenza. Additionally, if mutant strains continue emerging, spreading, and become resistant to current vaccines, then more booster vaccines will be needed as is the case for immunizing against influenza. Additionally, other vaccine types such as intranasal formulations or a universal coronavirus vaccine should be explored that could provide more durable immunity. The virus might continue to cause mild illness for some and more serious illness for others, depending on their overall health, vaccine status and prior infections. But in this scenario, society is open and people are working, attending school and social events.

What is COVID-19 "long-hauler" syndrome?
Click for more infoWhat is COVID-19 "long-hauler" syndrome?
In the United States, 10% to 30% of people who had COVID-19 reported at least one moderate to a severe symptom that lasted more than two months are referred to as post-COVID “long haulers.” Recent studies (see here and here), as well as surveys conducted by patient groups, suggest that 50% to 80% of patients continue to have bothersome symptoms even after tests can no longer detect virus in their body for up to three months after the initial onset of COVID-19. More than 200 symptoms have been reported with the most common ones including fatigue, body aches, shortness of breath, difficulty concentrating, inability to exercise, headache, and difficulty sleeping. There can also be dermatological manifestations such as the emergence of red or purple tender bumps on the toes or hands (“COVID toes”), along with a painful burning sensation in the skin. Since COVID-19 is a new disease that emerged for the first time in December 2019, long-term recovery rates are not yet available.
Most people who get COVID-19 recover within weeks or a few months. However, some may suffer chronic damage from the illness to their lungs, heart, kidneys or brain and experience persistent symptoms. In light of the rise of long COVID as a persistent and significant health issue, in July, 2021, the Office for Civil Rights in the U.S. Department of Health and Human Services and the Civil Rights Division of the U.S. Department of Justice determined that long COVID can be considered a disability under the Americans with Disabilities Act, paving the way for some people suffering from the chronic effects of COVID-19 to receive accommodations from businesses, schools and employers.
Additional Information Resources
Additional Information Resources
CDC Information on Post-COVID Conditions
Guidance on “Long COVID” as a Disability Under the ADA

I have been fully vaccinated. What can I now do safely?
Click for more infoI have been fully vaccinated. What can I now do safely?
If you are fully vaccinated and have received a booster, you can resume many of the activities you had stopped doing because of pandemic. Be sure to follow Federal, State and local public health guidance. Recent research has revealed that vaccinated people can still transmit the virus to other people so it is advisable to wear masks indoors in areas of the country where the coronavirus is spreading and in certain other settings including while on public transportation. Schools, workplaces and businesses may require mask wearing as well regardless of vaccination status.
Fully vaccinated people might choose to wear a mask regardless of the level of transmission, particularly if they are immunocompromised or at increased risk for severe disease from COVID-19, or if they have someone in their household who is immunocompromised, at increased risk of severe disease or not fully vaccinated. How long vaccine protection lasts and how much vaccines protect against emerging SARS-CoV-2 variants are still under investigation.
Because it takes time for your body to build protection after vaccination, you’re considered fully vaccinated two weeks following immunization. For COVID-19 vaccines that require two shots, you should wait to resume activities until about two weeks after your second vaccination. For COVID-19 vaccines that require one shot in the initial dosing, you should wait about 2 weeks after vaccination for your body to build protection and to resume usual activities. Studies shown that from seven days onward, booster vaccines are extremely effective at preventing illness from COVID-19. See CDC guidance below for fully vaccinated individuals:
- You can resume activities, without wearing a mask or staying 6 feet apart, except indoors where COVID-19 infections are rapidly spreading and where required by federal, state, local, tribal, or territorial laws, rules, and regulations, including local business, workplace, and school guidance.
- You can now travel within the United States without getting tested before or after travel, .
- You will not need to get tested before leaving the United States for international travel unless it is required by the destination. You will not have to self-quarantine after arriving back in the United States if you are fully vaccinated. If you’ve been around someone who has COVID-19, you should get tested 5 days after your exposure, even if you don’t have symptoms. You should also wear a mask indoors in public for 10 days following exposure or until your test result is negative. You should isolate for 5 days if your test result is positive and wear a mask for 10 days once you test negative..
Additional Information Resources
Guidance for When You Have Been Fully Vaccinated
Because it takes time for your body to build protection after vaccination, you’re considered fully vaccinated two weeks following immunization. For COVID-19 vaccines that require two shots, you should wait to resume activities until about two weeks after your second vaccination. For COVID-19 vaccines that require one shot, you should wait about 2 weeks after vaccination for your body to build protection and to resume usual activities. Studies shown that from seven days onward, booster vaccines are extremely effective at preventing illness from COVID-19. See CDC guidance below for fully vaccinated individuals:
- You can resume activities, without wearing a mask or staying 6 feet apart, except indoors where COVID-19 infections are rapidly spreading and where required by federal, state, local, tribal, or territorial laws, rules, and regulations, including local business, workplace, and school guidance.
- You can travel within the United States without getting tested before or after travel and without self-quarantining after travel in most states and cities.
- You will not need to get tested before leaving the United States for international travel unless it is required by the destination. You will not have to self-quarantine after arriving back in the United States if you are fully vaccinated. If you’ve been around someone who has COVID-19, you should get tested 3-5 days after your exposure, even if you don’t have symptoms. You should also wear a mask indoors in public for 14 days following exposure or until your test result is negative. You should isolate for 10 days if your test result is positive.
Additional Information Resources
Mythbusters for COVID-19
Click for more infoMythbusters for COVID-19
To help dispel some common misconceptions about COVID-19, the World Health Organization established a website to combat the most common myths about the disease.

Have a COVID-19 question?
Click for more infoHave a COVID-19 question?
The Johns Hopkins Bloomberg School of Public Health (JHU) has launched a free interactive tool to help answer the public’s questions on the COVID-19 virus. To use this service, type in a question. If you don’t find the answer, you can email PublicHealthQuestion@jhu.edu and receive a response from researchers at the JHU School of Public Health. Visit the site here.
Find answers to your questions about COVID-19 and vaccines from the CDC here.

How can we protect kids from COVID-19?
Click for more infoHow can we protect kids from COVID-19?
The risk of children becoming infected with COVID-19 is on the rise. As of Jan 12, 2023, almost 15.3 million children are reported to have tested positive for COVID-19 since the beginning of the pandemic. Although most will experience mild symptoms, there are reports of kids becoming critically ill. Children over the age of 6 months are eligible for immunization Take the following precautions to reduce the risk of your child getting infected with COVID-19:
- Vaccinate your child over the age of 6 months against COVID-19. Follow the CDC guidelines for boosters based on their age.
- All eligible people in a child’s household should get immunized. An important strategy to protect children from COVID-19 is to have all of their close contacts vaccinated. All adults and siblings over the age of 6 months should get immunized. COVID-19 vaccines reduce the risk of people getting COVID-19 and can also reduce the risk of spreading it to others including children.
- Socialize and play outdoors. Risk of outdoor transmission of COVID-19 remains relatively low. CDC guidelines state that unvaccinated individuals can participate in outdoor activities without masking. Therefore, it is important during this surge to convene social gatherings outside as a precaution whenever possible. If you are indoors, choose a location that is well ventilated, e.g. a room with open windows and use masks if you are in an area where the virus is spreading whenever possible.
- Masking indoors when around unvaccinated people or in crowded public settings is advisable in areas where the virus is spreading. Consider having everyone in your family, even those who are vaccinated, wear a mask indoors in crowded public spaces like public transportation if you are in an area where the virus is spreading. Most counties in the United States are now experiencing a rise in infections. Provide a well-fitted, high-quality mask for your child and have them wear it.
- Create pandemic pods to reduce the risk of exposure. Form a small group that you coordinate with your child’s after-school activities or carpools to minimize the number of individuals kids come into contact with.
- Stay vigilant even during informal events. It’s easy to let your guard down when you’re trying to enjoy milestones or moments with you kids. Stay consistent with putting into practice public health guidance to minimize the risk of contracting COVID-19 as well as to make this a routine for children. Additional Information Resources
COVID-19 Parental Resources Kit
Know What to Expect at Your Child’s K- 12 School or Child Care Program
- Mask indoors when around other unvaccinated people or in public. Have everyone in your family, even those who are vaccinated, wear a mask indoors in public if you are in an area where the virus is spreading. Most counties in the United States are now experiencing a rise in infections. Provide a well-fitted, high-quality mask for your child and have them wear it. If necessary, discuss with other parents about the need to mask up inside in order to protect young people.
- Create pandemic pods to reduce the risk of exposure. Form a small group that you coordinate with your child’s after-school activities or carpools to minimize the number of individuals kids come into contact with. Adopt the same preventative strategies in your group, e.g. masking indoors and social distancing where needed.
- Stay vigilant even during informal events. It’s easy to let your guard down when you’re trying to enjoy milestones or moments with you kids. Stay consistent with putting into practice public health guidance to minimize the risk of contracting COVID-19 as well as to make this a routine for children. Avoid crowded places and gatherings where it may be hard to stay at least 6 feet away from others who don’t live with you.
Additional Information Resources
COVID-19 Parental Resources Kit
Know What to Expect at Your Child’s K- 12 School or Child Care Program

Can I get COVID from swimming in a pool?
Click for more infoCan I get COVID from swimming in a pool?
The CDC is not aware of any scientific reports of the virus that causes COVID-19 spreading to people through the water in pools, hot tubs, water playgrounds, or other treated aquatic venues. Check with your local municipality to see guidelines for pool access. SARS-CoV-2, the virus that causes COVID-19, most commonly spreads from person-to-person by respiratory droplets during close physical contact (within 6 feet or a few inches longer than a typical pool noodle, both in and out of the water). The virus can sometimes spread from person-to-person by small droplets or virus particles that linger in the air for minutes to hours. This can happen most easily in enclosed spaces with inadequate ventilation. In general, being outdoors and in spaces with good ventilation reduces the risk of exposure to infectious respiratory droplets.
Ways to promote behaviors that prevent the spread of COVID-19 include:
- Those who are not fully vaccinated should wear masks consistently and correctly, but they should not wear them in the water. They should also avoid sharing items that are meant to come in contact with the face (such as goggles, nose clips, and snorkels) which are not substitutes for masks.
- Unvaccinated individuals should also practice social distancing staying 6-feet away from people they don’t live with. This includes not gathering at the ends of swim lanes, behind starting blocks, or on stairs into the water or up to the diving board.
- Wash your hands with soap and water for at least 20 seconds. If soap and water are not readily available. Do not to spit and to cover coughs and sneezes with a tissue or use the inside of their elbows, throw used tissues in the trash, and wash their hands immediately with soap and water for at least 20 seconds. Use hand sanitizer that contains at least 60% alcohol, if soap and water are not readily available.
Is the COVID-19 vaccine safe?
Click for more infoIs the COVID-19 vaccine safe?
Yes, more than 13 billion doses of COVID-19 vaccines had been administered in the United States from December 14, 2020, through January 28, 2023 (https://ourworldindata.org/covid-vaccinations). COVID-19 vaccines were evaluated in tens of thousands of participants in clinical trials. The vaccines met the Food and Drug Administration’s (FDA’s) rigorous scientific standards for safety, effectiveness, and manufacturing quality needed to support emergency use authorization (EUA). The Pfizer/BioNTech and Moderna COVID-19 vaccines have received full approval from FDA. The COVID-19 vaccines will continue to undergo the most intensive safety monitoring in US history. This monitoring includes using both established and new safety monitoring systems to make sure that COVID-19 vaccines are safe and effective.
What is the Test-To-Treat Initiative?
Click for more infoWhat is the Test-To-Treat Initiative?
As part of President Biden’s National COVID-19 Preparedness Plan to help America move forward safely, the Administration has launched a nationwide Test to Treat Initiative that allows Americans to rapidly access needed COVID-19 at home treatments. Through this program, people who test positive for COVID-19 will be able to visit hundreds of local pharmacy-based clinics and federally-qualified community health centers (FHQCs), and residents of long-term care facilities will in one stop, be assessed by a qualified health care provider who can prescribe antiviral pills on the spot. This ensures that, if people who are at high risk for developing severe disease test positive and if administration of an antiviral is appropriate, they can get treatment quickly and easily. The program is run by the U.S. Department of Health and Human Services (HHS) and includes a direct allocation of antiviral pills to participating clinics, centers, and facilities.
In January 2023, the NIH in collaboration with ASPR, launched the Home Test to Treat Program, an entirely virtual community health intervention that will provide free COVID 19 health services- at home rapid test, telehealth session and at home treatments- in selected communities. It will make antiviral treatment available for eligible individuals who receive a positive test result, which could help prevent severe illness, hospitalization or death. Home Test to Treat will promote equitable solutions and help to identify best practices that may save lives in this and future pandemics.
The steps included in this initiative are:
- Get Tested for COVID-19 at a Test to Treat site or bring your test results from an at-home test, a pharmacy or your health care provider with you to your visit.
- Get a prescription from an on-site healthcare provider if you are at high risk of getting very sic
- Get Treated – Ask the on-site or affiliated pharmacist to fill the prescription
If you are participating in the Home Test to Treat program being implemented in selected communities, you will receive these services virtually
Learn more here.
Access Frequently Asked Questions here.
The steps included in this initiative are:
- Get Tested for COVID-19 at a Test to Treat site or bring your test results from an at-home test, a pharmacy or your health care provider with you to your visit.
- Get a prescription from an on-site healthcare provider if you are at high risk of getting very sic
- Get Treated – Ask the on-site or affiliated pharmacist to fill the prescription
Learn more here.
Access Frequently Asked Questions here.
